How to Reduce Redness on Face: The Neurosensory Approach to Sensitive Skin (2025 Guide)
It starts with a flush that doesn’t go away. Then comes the heat—a prickly, uncomfortable warmth that feels less like “dry skin” and more like an invisible sunburn. If you are reading this, you’ve probably tried the heavy creams, the “calming” masks, and the 10-step routines, only to find your face redder and angrier the next morning.
Here’s the thing: conventional advice often fails because it treats redness as a surface-level moisture problem. But for the 70% of us dealing with reactive skin, the issue runs deeper. It’s neurosensory.
In my years of researching skin barrier function, I’ve found that chronic redness is rarely just about dry patches. It’s a signaling error between your nerves and your blood vessels. This article isn’t just about covering it up; it’s about extinguishing the fire at the source.
The estimated size of the sensitive skin care market in 2023, projected to nearly double by 2030, proving you are not alone in this struggle.
Source: Grand View Research (2024)
We are going to move beyond basic tips and dive into the specific biological mechanisms of how to reduce redness on face, utilizing the latest 2025 research on neurosensory skin dysfunction. Let’s get your skin back to baseline.
The “Invisible Burning” Syndrome: Why Your Skin is Actually Red
Before we can fix the redness, we have to understand the mechanism. Why does your face get red and hot randomly? It’s easy to blame the weather or that glass of wine, but the physiological trigger is specific.
Sensitive vs. Sensitized: Knowing the Difference
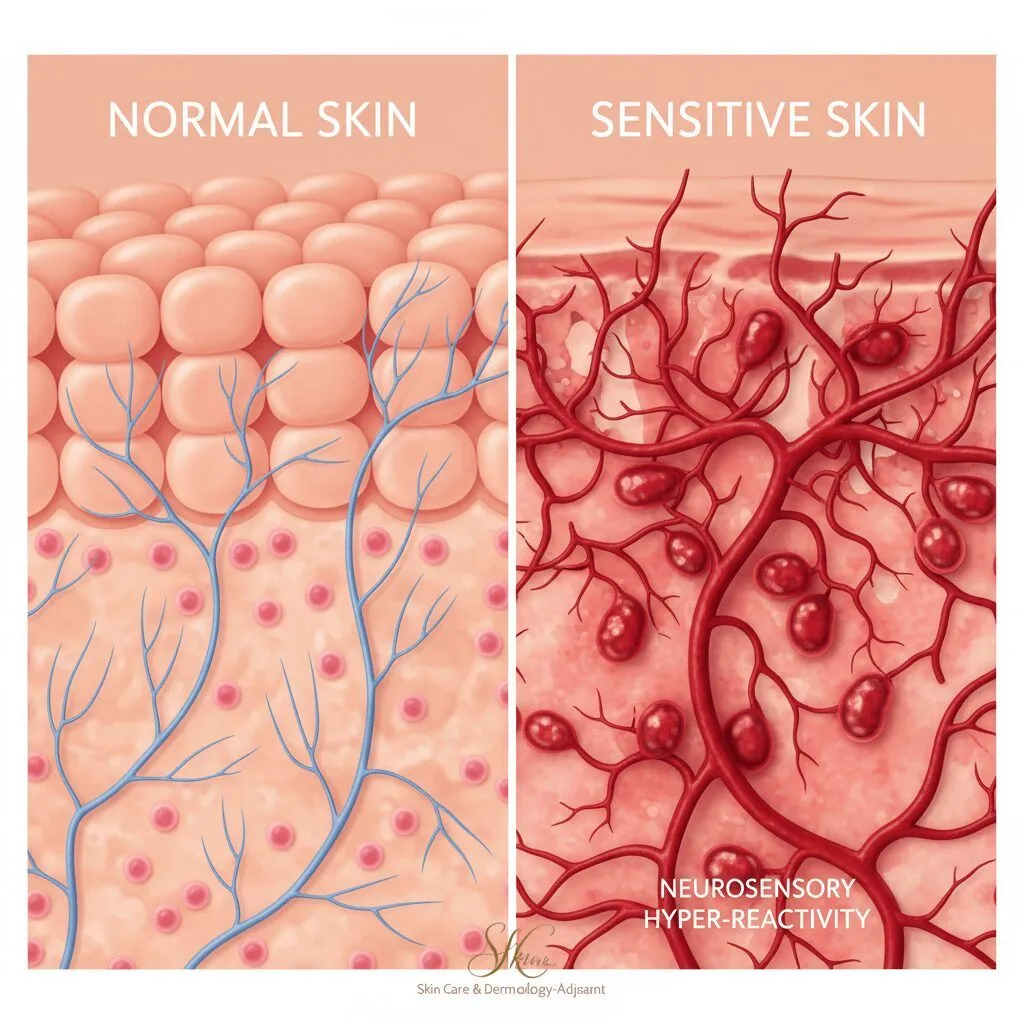
There is a distinct difference between skin type and skin condition. Sensitive skin is genetic—you were likely born with a thinner stratum corneum (outer layer) and blood vessels that sit closer to the surface. Sensitized skin, however, is a temporary condition caused by external aggressors like over-exfoliation, pollution, or harsh ingredients.
Dr. Jenny Liu, a Board-Certified Dermatologist, explains this nuance perfectly in her recent breakdown of rosacea-prone skin: “Sensitive skin is different from sensitized skin, but when skin barrier is compromised these products can help… Start off slow and low [with actives].” (Dr. Jenny Liu, May 2025).
If your redness is accompanied by stinging when you apply water, you are likely sensitized—meaning your barrier is damaged. If you flush easily but the barrier is intact, you are likely sensitive or dealing with rosacea.
The Neurosensory Connection: TRPV1 Receptors
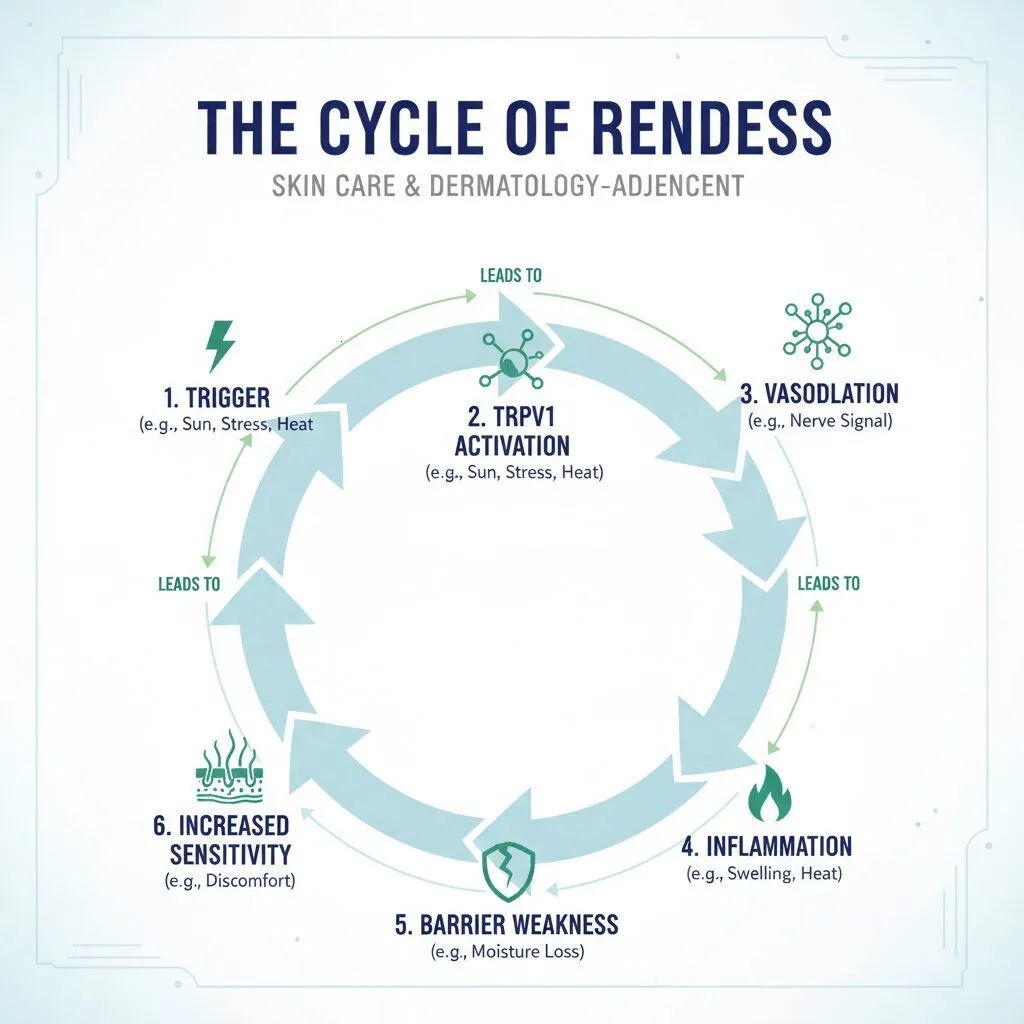
This is the science most blogs miss. Your skin contains transient receptor potential vanilloid 1 (TRPV1) receptors. Think of these as your skin’s smoke detectors. In normal skin, they only go off when there is actual heat or damage.
In red, prone-to-flushing skin, these receptors are hyper-reactive. They perceive harmless triggers (like lukewarm water, spicy food, or even stress) as a threat, causing the nervous system to flood the area with blood to “heal” the perceived injury. This vascular dilation causes the redness.
The Role of “Inflammaging” in Chronic Redness
A new term dominating the 2025 skincare conversation is “Inflammaging”—chronic, low-grade inflammation that accelerates aging and keeps skin permanently flushed. Dr. Dendy Engelman notes in a report from Good Housekeeping (Sept 2024): “Redness is inflammation, which causes tiny blood vessels to expand and push against the skin… Dry skin is often damaged and compromised, which means that skin becomes vulnerable to infection.”
When you ignore redness, you aren’t just dealing with a cosmetic issue; you are allowing chronic inflammation to degrade your collagen.
Immediate Triage: How to Calm Redness in 20 Minutes
Sometimes you don’t have weeks to repair your barrier. You need the red out now. Here are the fastest, non-damaging ways to reduce facial erythema immediately.
The “Thermal Water” Evaporation Method
Many people spray thermal water and let it air dry. Do not do this. As the water evaporates, it draws moisture out of your skin (TEWL), leaving you tighter and redder.
The Correct Protocol:
- Generously mist the face with thermal spring water (rich in selenium or silica).
- Let it sit for exactly 30 seconds to cool the skin surface.
- Gently blot (don’t rub) the excess with a tissue.
- Immediately apply a humectant moisturizer while the skin is still damp to seal in the hydration.
Green Theory: Using Color Correctors without Clogging
Green sits opposite red on the color wheel, neutralizing it. However, many green primers are loaded with silicones that trap heat—the enemy of rosacea. Look for “serum-based” color correctors containing Centella Asiatica (Tiger Grass). These treat the redness while covering it, rather than just masking it.
The “Zero-Friction” Cleansing Technique
Mechanical friction is the number one trigger for morning redness. If you use a washcloth, scrub, or cleansing brush, stop immediately. Switch to a “cushion cleanse” method: use enough oil or milk cleanser that your fingers glide over your face without actually pulling the skin. Rinse with cool—never hot—water.
The 3-Step Barrier Repair Protocol (Science-Backed)
To permanently reduce redness, we have to rebuild the roof of the house (the stratum corneum). Based on current dermatological consensus, this is the gold-standard protocol.
Step 1: Lipid Replacement (Ceramides & Squalane)
Your skin barrier is a brick wall. The cells are the bricks, and the “mortar” holding them together consists of ceramides, cholesterol, and fatty acids. When you strip this mortar, the wall crumbles, and irritants get in.
According to Journal of Drugs in Dermatology (Jan 2024), while 60-80% of sensitive skin patients see a dermatologist, the solution often starts at home with lipid replenishment. Look for moisturizers containing Ceramide NP, AP, and EOP paired with Squalane, which mimics the skin’s natural oils.
Step 2: The “Fire Extinguishers” (Centella Asiatica)
If lipids rebuild the wall, Centella Asiatica puts out the fire burning inside the house. This ancient herb has massive clinical backing in 2025.
A 2024 clinical trial published in the Journal of Cosmetic Dermatology found that mean sensitive skin scores dropped by 66% after just 2 weeks of using Centella Asiatica. It significantly reduced irritation, tautness, itching, and redness.
In my experience, products labeled “Cica” (short for Centella) are non-negotiable for redness prone skin. They downregulate the inflammatory markers that cause the flush.
Step 3: Microbiome Balancing
Your skin has an ecosystem of bacteria. Harsh cleansers kill the good guys, allowing Staphylococcus aureus to overgrow, which drives inflammation. Regina Heng, an industry expert with Cetaphil, noted in a forecast for CosmeticsDesign-Asia (Nov 2025) that there is “increasing demand for formulations that are gentle yet effective, bridging the gap between prevention and protection.” This means using prebiotic skincare to feed the good bacteria that keep your skin calm.

Ingredient Deep Dive: What Works & What Burns
Navigating an ingredient label can feel like reading a foreign language. Let’s simplify it. Here is what you need to look for, and more importantly, what to avoid.
Niacinamide: The 5% vs. 10% Trap
Niacinamide (Vitamin B3) is everywhere. It strengthens the barrier and brightens skin. However, there is a dangerous trend of high-percentage serums (10-20%).
Clinical data referenced in recent 2024 analyses indicates that the “sweet spot” for Niacinamide is 2% to 5%. At this level, it boosts ceramide production by 67%. Once you cross into 10% territory, it can trigger histamine responses in sensitive users, actually causing the redness you are trying to treat. If a product burns when you apply it, check the niacinamide percentage.
Azelaic Acid: The Gold Standard for Erythema
If you have Rosacea or persistent redness, Azelaic Acid is your best friend. Unlike retinoids, which can be harsh, Azelaic Acid is an anti-inflammatory that kills the bacteria associated with rosacea and calms the vascular response. It is one of the few actives that dermatologists recommend using even during a flare-up.
The “No-Go” List
According to Dr. Lycia Thornburg of the American Academy of Dermatology, “It’s possible to control your rosacea and even prevent it from getting worse by recognizing and avoiding triggers.” Here are the top offenders I see clients using by mistake:
| Ingredient | Why it triggers redness | Safe Alternative |
|---|---|---|
| Alcohol Denat / SD Alcohol | Strips lipids, destroys barrier, causes immediate vasodilation. | Fatty Alcohols (Cetyl, Stearyl) |
| Witch Hazel | Often distilled in alcohol; high tannin content can be astringent and drying. | Rose Water or Mugwort |
| Essential Oils (Lavender, Peppermint) | Volatile compounds that trigger allergic contact dermatitis. | Bisabolol or Allantoin |
| Glycolic Acid (High %) | Small molecular size penetrates too fast, stinging nerves. | Lactic Acid or PHA (Polyhydroxy Acid) |

Lifestyle Factors: The “Inside-Out” Redness Triggers
You can use the best cream in the world, but if your internal environment is inflamed, your skin will show it. The skin is a window into the body’s stress levels.
Histamine-Rich Foods and the “Flush” Effect
Have you ever noticed your face gets hot after eating aged cheese, drinking red wine, or eating spicy food? This is a histamine response. For those with compromised barriers, the body lacks the enzyme (DAO) to break down histamine efficiently. This leads to vascular dilation (flushing). Keeping a food diary can be a game-changer.
Stress & Cortisol: Managing “Cortisol Face”
This is a major topic for 2025. “Cortisol Face” refers to the puffiness and redness induced by chronic stress. High cortisol levels weaken the skin barrier and increase pro-inflammatory cytokines.
A trend report from Beauty Independent (Jan 2025) highlights that consumers are now recognizing inflammation is the root cause of aging. Managing stress—through vagus nerve cooling exercises or meditation—is now considered a legitimate part of a skincare routine.
Vitamin D and Immunity
Interestingly, a 2025 meta-analysis discussed the relationship between Vitamin D status and immune response. Adequate Vitamin D3 levels are crucial for skin immunity. A deficiency can leave the skin barrier weak and unable to defend against environmental triggers.
FAQ: Dermatologist Solutions to Common Problems
Q: What is the fastest way to get rid of face redness?
A: For immediate relief, use a cold compress (not ice directly on skin) for 10 minutes to constrict blood vessels, followed by a Centella Asiatica serum. Avoid covering it with heavy makeup immediately, which can trap heat.
Q: Does drinking water help reduce skin redness?
A: Indirectly, yes. Dehydration creates a “prune” effect, making fine lines and redness more visible. However, drinking water alone won’t fix a broken barrier; you need topical hydration (humectants) + occlusion (lipids) to hold that water in.
Q: Why does niacinamide burn my face?
A: As mentioned earlier, your concentration is likely too high. Switch to a product with 2-5% Niacinamide. If it still burns, your barrier may be too damaged for any actives. Switch to pure bland moisturizers (petrolatum or dimethicone based) until the skin heals.
Q: Can stress cause permanent facial redness?
A: Chronic stress causes chronic inflammation. Over time, repeated flushing (vasodilation) can cause the capillaries to lose their elasticity and remain permanently dilated (telangiectasia), which is a hallmark of rosacea.
Conclusion
Reducing redness on the face is not about finding a miracle “erasing” cream. It is about understanding that your skin is communicating with you. That heat, that flush, and that irritation are signs of a neurosensory system on high alert.
To tame the redness, remember the three pillars we discussed:
- Repair the Barrier: Use ceramides and squalane to rebuild the wall.
- Calm the Nerves: Utilize ingredients like Centella Asiatica and low-percentage Niacinamide to soothe the “fire.”
- Eliminate Triggers: Watch out for alcohol, hot water, and histamine-rich foods.
Healing a compromised barrier takes time—usually about 28 days for a full skin cycle. Be patient, be gentle, and stop fighting your skin. Start nourishing it instead.
