Top Acne Treatments That Actually Work: The New 2025 Dermatologist Guidelines
Let’s be honest for a second: if scrolling through TikTok trended your way to clear skin, you wouldn’t be reading this right now. You’d be out enjoying your complexion. But instead, you’re likely frustrated, confused by conflicting advice, and tired of spending money on products that promise the moon but deliver more irritation.
I’ve been there. In my years covering dermatological advancements, I’ve noticed a pattern: most people are treating 2025 acne with 2010 protocols. But the game has changed.
For the first time in eight years, the American Academy of Dermatology (AAD) has updated its official guidelines. We have moved past the era of simply “drying it out.” The new science of clear skin is about multimodal therapy, microbiome preservation, and high-tech interventions that target the sebaceous glands directly.
According to Pierre Fabre Laboratories, acne affects approximately 20.5% of the global population over age 16. It is not just a teenage phase; it is a medical condition that requires a medical strategy. This article isn’t a list of random creams—it is your definitive roadmap to the treatments that actually work, backed by the absolute latest data from 2024 and 2025.
Content Roadmap:
1. Understanding Your Acne Type (The Diagnostic Step)
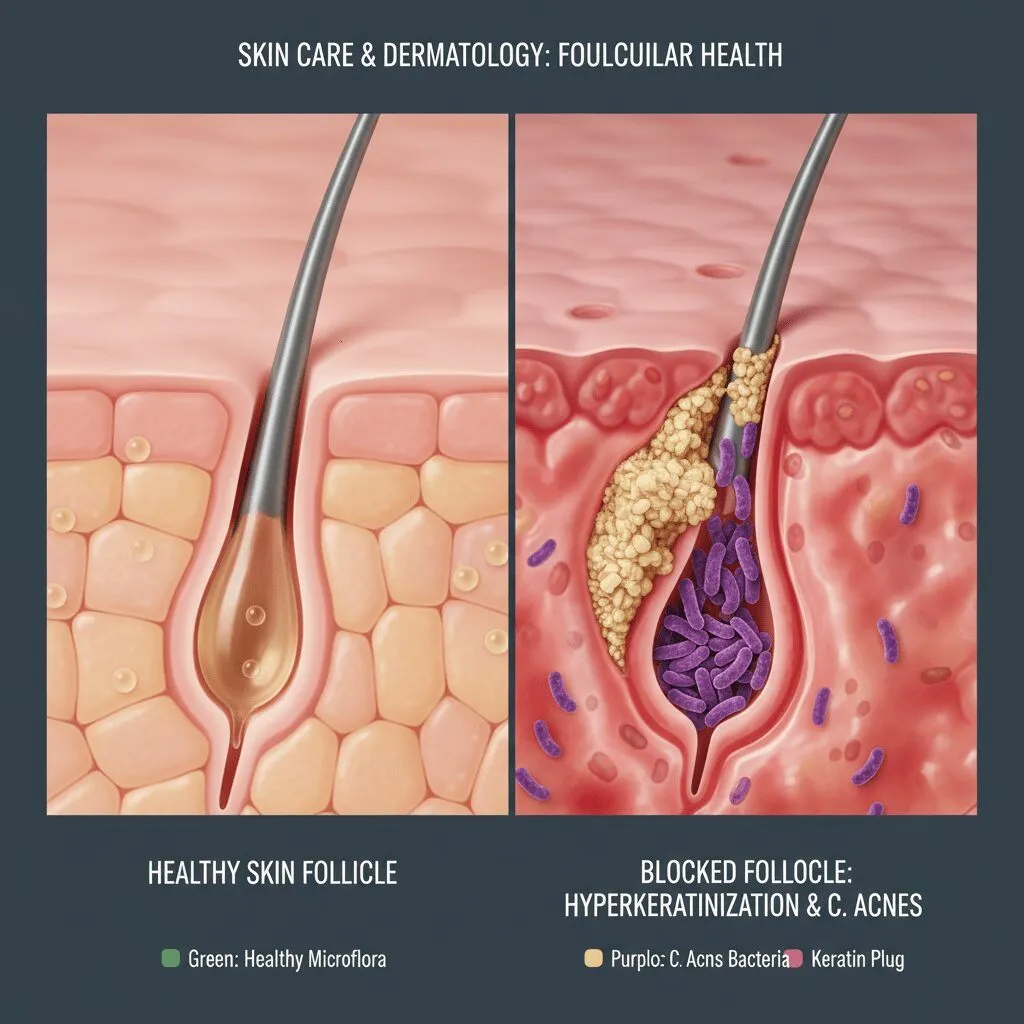
Before we discuss solutions, we must define the problem. You cannot treat hormonal cysts with a blackhead scrub—it simply won’t work. Acne is a disorder of the pilosebaceous unit (hair follicle and oil gland), but it manifests in different ways.
In my opinion, the biggest mistake people make is treating all bumps the same. Here is how to map your face according to the latest medical consensus:
Inflammatory vs. Non-Inflammatory (Comedonal)
Comedonal Acne: These are your whiteheads and blackheads. They are non-inflammatory plugs of sebum and dead skin cells. If your skin feels like sandpaper but isn’t red or painful, this is you. The primary culprit here is hyperkeratinization—your skin cells aren’t shedding correctly.
Inflammatory Acne: This happens when the C. acnes bacteria (formerly P. acnes) colonizes that clogged pore, triggering an immune response. This leads to papules (red bumps), pustules (pus-filled), and cysts (deep, painful nodules). According to the AAD Guidelines 2024, moderate-to-severe inflammatory acne leads to scarring in 30% to 95% of patients, making early, aggressive intervention critical.
Hormonal Acne Mapping
If your breakouts are concentrated along the jawline, chin, and lower cheek, and they flare up cyclically, you are likely dealing with hormonal acne. This is statistically more common in adult women.
“Women are significantly more affected than men in adulthood, with a 23.6% prevalence rate versus 17.5% for men,” according to a March 2024 report from Pierre Fabre Laboratories.
Recognizing this pattern is vital because standard topical antibiotics often fail here; you need to address the androgen receptors (more on Clascoterone later).
2. The New “Gold Standard” Topicals (2025 Updates)
This is where the landscape has shifted most dramatically. If you last saw a dermatologist in 2018, your prescription is likely outdated.
— Dr. John S. Barbieri, MD, MBA, FAAD, Co-chair AAD Acne Guideline Workgroup (AAD Press Release, Jan 31, 2024)
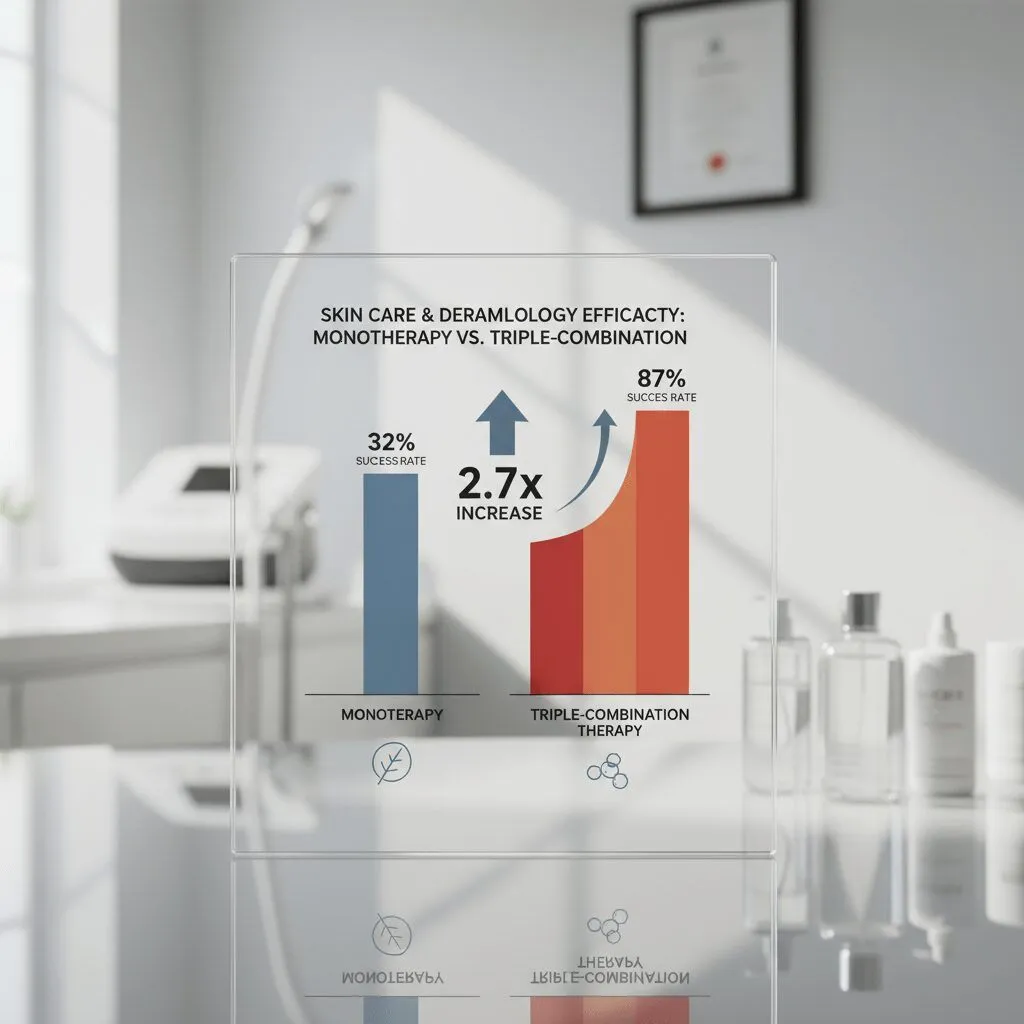
The “Triple Threat”: Clindamycin + Benzoyl Peroxide + Adapalene
For years, we had to layer three different creams. Now, science has stabilized them into fixed-dose combinations. The most notable advancement is the approval of the first triple-combination topical (IDP-126).
Why does this matter? It attacks acne from three angles simultaneously:
- Benzoyl Peroxide: Kills bacteria.
- Clindamycin: Reduces inflammation.
- Adapalene: Unclogs pores and normalizes cell turnover.
The results are statistically undeniable. According to MDedge analysis of the AAD Guidelines, this triple combination therapy showed a 2.19 times greater likelihood of success compared to the vehicle (placebo). Furthermore, data from Bausch Health regarding IDP-126 indicates that 50% of participants achieved “clear” or “almost clear” status by Week 12.
Clascoterone (Winlevi): The Hormonal Game-Changer
For decades, if you had hormonal acne, your only real options were oral birth control or Spironolactone pills. That changed with Clascoterone cream 1%.
It is the first topical androgen receptor inhibitor. Think of it as a shield for your oil glands. It doesn’t change your body’s systemic hormones; it simply blocks the “acne signal” at the skin level.
According to a systematic review published by the NIH in April 2024, Clascoterone 1% cream showed success rates of 18.4% versus 9.0% for placebo. While those numbers might look modest, for patients who cannot take oral hormones, this is a revolutionary tool.
— Dr. Bunick & Dr. Issa, writing for Dermatology Times (Feb 2, 2024)
Why Antibiotics Are No Longer Used Alone
One of the strongest directives from the 2024 AAD Guidelines is the stance on antibiotic stewardship. Topical antibiotics (like plain clindamycin gel) are strongly recommended against as monotherapy due to resistance risks (AAD Guidelines 2024).
If you are using a topical antibiotic, you must pair it with benzoyl peroxide to prevent the bacteria from mutating and becoming resistant. It’s not just about your skin; it’s about global health.
3. Over-The-Counter Heroes: What Still Works
Not everyone needs a prescription. If you are dealing with mild-to-moderate acne, the drugstore aisle holds powerful solutions—if you pick the right ones.
Benzoyl Peroxide: Less is More
There is a persistent myth that 10% Benzoyl Peroxide (BP) is better than 2.5%. This is false. High concentrations increase irritation, which damages the skin barrier and can actually induce more acne.
The goal is to kill bacteria, not burn your face off. A 2.5% to 5% wash, left on the skin for 2-3 minutes before rinsing (contact therapy), is the sweet spot. It minimizes irritation while delivering the antibacterial benefit.
Retinoids: Adapalene vs. Retinol
If you have comedonal acne (clogged pores), retinoids are non-negotiable. But which one?
Adapalene (Differin): This is the only prescription-strength retinoid available OTC in the US. It is specifically studied for acne.
— Dr. Andrea L. Zaenglein, MD, Penn State University (MDedge, March 13, 2024)
Retinol: Generally too weak for active acne. It’s better suited for anti-aging. Stick to Adapalene for breakouts.
Azelaic Acid: The Multi-Tasker
For those with sensitive skin or Rosacea-prone acne, Azelaic Acid is a powerhouse. It kills bacteria, reduces redness, and fades dark spots (Post-Inflammatory Hyperpigmentation). According to an NIH Systematic Review (April 2024), Azelaic acid gel reduced mean Total Lesion Count by 60.6% compared to 19.9% with placebo.
4. Systemic Treatments: When Creams Aren’t Enough
Sometimes, the root cause is too deep for a cream to reach. Systemic therapy is often required for nodulocystic acne or acne that is scarring.
Isotretinoin (Accutane): Still the Nuclear Option
Despite the fear-mongering online, oral isotretinoin remains the single most effective cure for severe acne. It is the only drug that permanently shrinks sebaceous glands.
A meta-analysis from the Annals of Family Medicine (Jan 2024) confirms that oral isotretinoin has a relative lesion reduction of 48.4% compared to other standard therapies. The success rate is high, but the side effects (dryness, birth defects risk) require strict monitoring.
Spironolactone: The Hormonal Hero for Women
I’ve seen Spironolactone change lives for women suffering from “chin cysts.” It is a diuretic that has an off-label benefit of blocking androgen receptors. The AAD 2024 guidelines have solidified its place as a preferred treatment for adult female acne, often sparing women from needing antibiotics.
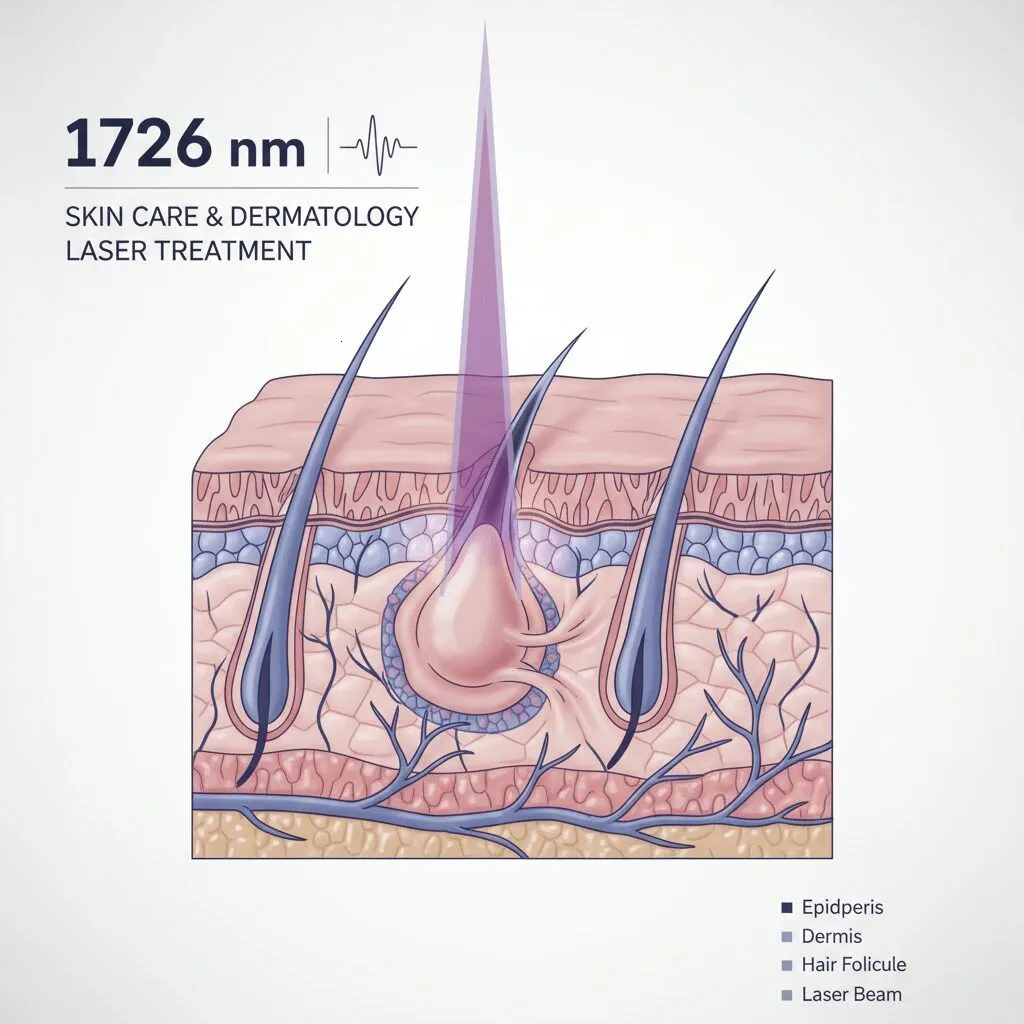
5. The Future is Here: 1726 nm Lasers (AviClear/Accure)
This is the most exciting development I’ve seen in my career for those seeking a “drug-free” cure. Until recently, lasers were mostly for scarring. Now, we have lasers specifically designed to target and suppress the sebaceous gland itself.
The 1726 nm wavelength (found in devices like AviClear) bypasses the skin’s surface and selectively heats the oil gland. It essentially “cooks” the acne factory without damaging the surrounding tissue.
According to Dermsquared (citing clinical trials, Jan 16, 2025), approximately 80% of patients experience at least a 50% reduction in inflammatory lesions with these new laser therapies. Furthermore, about 40% of patients achieve clear or almost clear skin 6 months post-treatment.
The downside? Cost. These treatments can range from $3,000 to $4,000 for a series and are rarely covered by insurance. However, for those who cannot take Accutane, this is a viable permanent alternative.
6. The “Skin Barrier” Factor (Crucial Missing Link)
You can have the best medication in the world, but if your skin barrier is compromised, you will not clear up. In fact, you will get worse. This is a phenomenon known as acne mechanica or irritant contact dermatitis mimicking acne.
When you use harsh acids and retinoids, you strip the lipids that hold your skin cells together. Bacteria can then penetrate easier, causing more inflammation. It’s a vicious cycle.
The Repair Protocol
The 2025 approach is “Barrier First.” This means integrating ceramides and hydration alongside your actives.
- Step 1: Use a non-foaming, hydrating cleanser in the morning.
- Step 2: Apply a moisturizer containing ceramides or niacinamide before your retinoid (the “sandwich method”) if you are sensitive.
- Step 3: Never skip sunscreen. UV rays inflame the skin and darken acne scars.
This aligns with data on the psychosocial impact of acne. A Pierre Fabre Global Study (March 2024) found that 50% of acne sufferers report fatigue and 41% report difficulty sleeping due to the condition. Treating the skin gently helps reduce the visible redness that contributes to this distress.
7. Frequently Asked Questions
What is the absolute best treatment for hormonal acne in 2025?
Based on the 2024 AAD guidelines, the top tier treatment for hormonal acne involves a combination approach. For topical treatment, Clascoterone (Winlevi) is the only FDA-approved androgen inhibitor. For systemic treatment in women, oral Spironolactone is considered the gold standard. These tackle the hormonal root cause that antibiotics cannot reach.
How do I fix my damaged skin barrier from acne treatment?
If your skin is stinging or extremely red, stop all “active” treatments (retinoids, acids, BP) for 5 to 7 days. Focus entirely on hydration using products rich in ceramides, hyaluronic acid, and panthenol. Once the stinging stops, reintroduce your acne treatments slowly, perhaps every other night, or use the “sandwich method” (moisturizer -> treatment -> moisturizer).
Is Benzoyl Peroxide or Salicylic Acid better?
It depends on your acne type. Benzoyl Peroxide is superior for inflammatory acne (red bumps/pustules) because it kills bacteria. Salicylic Acid is better for comedonal acne (blackheads/whiteheads) because it dissolves the oil plug. Many dermatologists recommend using a Salicylic Acid cleanser in the morning and a Benzoyl Peroxide spot treatment (or wash) at night, provided your skin can tolerate it.
Does drinking water actually help acne?
While staying hydrated is vital for overall health, there is no direct clinical evidence that drinking water “flushes out” acne. Acne is primarily caused by hormones, genetics, and follicular hyperkeratinization. However, severe dehydration can compromise the skin barrier, potentially worsening inflammation indirectly.
Conclusion: Your Clear Skin Roadmap
Acne is complex, but it is treatable. The “wait and see” approach is dead. With the 2024/2025 AAD Guidelines, we have a clear directive: treat early, treat with combination therapies, and protect the barrier.
Your Takeaway Steps:
- Identify your type: Is it inflammatory, comedonal, or hormonal?
- Start with the basics: A gentle cleanser, moisturizer, and sunscreen are the foundation.
- Add the actives: Incorporate Adapalene or Benzoyl Peroxide. Be patient—give it 12 weeks.
- Escalate if needed: If OTC fails, ask a dermatologist about the “Triple Combo” creams, Clascoterone, or Spironolactone.
You don’t have to live with acne. The science is on your side—you just need to use the right tools.
